Introduction
Background on the "Getting to Work" Educational Modules
Labour force participation and income support have been identified as critical issues facing the estimated 65,000 people living with HIV in Canada [1-2] . Recent studies suggest that approximately half of people living with HIV are unemployed [3-5]
. Recent studies suggest that approximately half of people living with HIV are unemployed [3-5] . While the links between health and labour force participation are complex, it is clear that labour force participation is an important social determinant of health.
. While the links between health and labour force participation are complex, it is clear that labour force participation is an important social determinant of health.
Organizations or individuals who work with people living with HIV can play a valuable role in assisting people living with HIV to make informed decisions about their employment options. These learning modules were developed to promote awareness and use of The HIV and Employment Framework (The Framework) among organizations and individuals engaged in employment work with people living with HIV [6] . Vocational rehabilitation workers, AIDS service organization staff and those working at other community agencies serving HIV positive people may find these modules particularly beneficial.
. Vocational rehabilitation workers, AIDS service organization staff and those working at other community agencies serving HIV positive people may find these modules particularly beneficial.
The Framework summarizes the available information on HIV and labour force participation and is based on a comprehensive review of the literature on HIV and employment from Canada and the United States [7] . To augment The Framework we conducted qualitative interviews, focus groups, and sought input from members of a community advisory committee comprised of individuals active in the HIV and employment fields, including people living with HIV.
. To augment The Framework we conducted qualitative interviews, focus groups, and sought input from members of a community advisory committee comprised of individuals active in the HIV and employment fields, including people living with HIV.
We then evaluated The Framework in focus groups as part of a Knowledge Translation study to promote and assess the use of The Framework and series of fact sheets among human resource professionals, vocational rehabilitation workers and AIDS service organization staff. To develop these educational modules, we received feedback from focus groups on the learning needs, applicability and appeal of the modules for vocational rehabilitation workers and AIDS service organization staff.
We hope you find this learning resource useful. HIV is considered to be an episodic illness (with periods of wellness followed by periods of illness), and the learning from these modules may help you not only in your work with people living with HIV, but also in work with people living with other episodic illnesses.
Introduction to the "Getting to Work" Learning Resource
This series of four modules is designed to provide any organization or individual engaged in employment work with people living with HIV with a background on key issues in labour force participation and return to work for people living with HIV.
Vocational rehabilitation workers, including counsellors, case managers and job developers, work with clients to prepare for, find, return to, change, maintain and exit employment. AIDS service organization staff may or may not deal directly with employment issues, but support and advocate for people living with HIV in variety of ways. Many other individuals are engaged in employment work with people living with HIV and we encourage all workers to consider their roles and share this learning with others. AIDS service organization staff may be able to provide more specific information related to human rights, disclosure, confidentiality and accommodation needs in the workplace. For a list of AIDS service organizations in your area, please visit ASO 411 [8] .
.
How to Use the Modules
This learning resource is comprised of four independent modules that feature key issues related to HIV and employment. You will see that each module includes an introduction, learning objectives, general questions, a case scenario, discussion questions, learning content, notes from experts and concludes with a section of resources. The general questions are the same for each case and apply to all modules. The discussion questions are unique and are specific to each case.
We have written this learning resource so that each module is a stand-alone resource; however, each one builds on the learning from the previous module, and thus we suggest that the modules be completed in numerical order.
We recommend that you complete the modules in small groups. Depending on their backgrounds and levels of experience, group members will bring different knowledge and skills to the discussions of the cases in each module. Learning with your colleagues can help to improve your collaboration and knowledge of other service providers. We have included guiding questions for individual reflection and small group discussion following each case. The ability to share and discuss perspectives and experiences is a benefit of small group learning, so we encourage you to share and learn about, from, and with each other.
We recommend that you schedule a one-hour session with your colleagues to complete each module. Please individually review the modules and the cases before each session with your colleagues. We suggest that you consider the general questions on your own and come prepared to discuss the discussion questions in the small group session with your colleagues. It is further suggested that you review the content and “From the Experts” comments to enhance your knowledge of the background on each case. Material in the “From the Experts” sections includes promising practices and tips from those experienced in the HIV and employment field, including members of the study’s Advisory Committee.
At certain places, you will see this symbol: ![]() . Clicking that symbol will allow you to see the references cited in that part of the text. All of the references for each Module can also be found under the "References" tab, as well.
. Clicking that symbol will allow you to see the references cited in that part of the text. All of the references for each Module can also be found under the "References" tab, as well.
Facilitator Role
These case scenarios work best if someone in the group volunteers to be the facilitator. The facilitator’s role is to promote discussion and encourage the group to go through the questions in the allotted time. You don’t need to be an expert in the topic areas to be a good facilitator.
As the facilitator, it is important to remind the participants to ask questions and to respect each other’s contributions to the learning experience. Please ensure that the importance of client confidentiality is discussed. You may wish to summarize for the group the key learning points at the end of the case discussion. If you are meeting regularly to go through the cases in sequence, you might want to rotate the facilitator role.
While this learning resource is intended to be applicable to many Canadian environments, each module can be adapted or modified to fit your local context. We would encourage you to consider any additional perspectives that affect your local health care and social service settings and communities.
References and Resources
- O' Brien, K., et al., Scoping the Field: Identifying Research Priorities in HIV and Rehabilitation, in Canadian Association of HIV/AIDS Research. 2008: Montreal. See conference poster at: http://www.hivandrehab.ca/EN/research/documents/Research-Priorities-Factsheet-June-08.pdf
- Public Health Agency of Canada, HIV/AIDS Epi Updates, July 2010. http://www.phac-aspc.gc.ca/aids-sida/publication/epi/2010/index-eng.php
- Worthington, C. and H.B. Krentz, Socio economic factors and health-related quality of life in adults living with HIV. International Journal of STD and AIDS, 2005. 16(9): p. 608-614. http://www.ncbi.nlm.nih.gov/pubmed/16176627
- Burgoyne, R.W. and D.S. Saunders, Perceived support in newly registered HIV/AIDS clinic outpatients. AIDS Care Psychological and Socio Medical Aspects of AIDS/HIV, 2000. 12(5): p. 643-650. http://www.ncbi.nlm.nih.gov/pubmed/11218549
- Cunningham, W., R. Anderson, and M. Katz, The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Medical Care, 1999.37: p. 1270-1281. http://www.ncbi.nlm.nih.gov/pubmed/10599608
- To access The Framework, additional fact sheets and information about the “Getting to Work” study, please visit http://gettingtowork.hivandrehab.ca/
- Worthington, O’Brien, Zack, Mckee & Oliver. Enhancing labour force participation for people living with HIV: A multi-perspective summary of research evidence. AIDS and Behaviour, 2011. 16(1): 231-243. doi: 10.1007/s10461-011-9986-y. http://www.ncbi.nlm.nih.gov/pubmed/21701906
- To locate an AIDS Service Organization or other HIV related organization in your area visit ASO 411. http://www.aso411.ca/
Acknowledgements
Educational Module leads: Patty Solomon and Lynne Sinclair, with Catherine Worthington, Kelly O’Brien, Sergio Rueda, Brent Oliver and Ashley Mollison.
Study team: Catherine Worthington (Principal Investigator, University of Victoria and University of Calgary), Martine Mangion (Principal Knowledge User, CWGHR), Melissa Popiel (CWGHR), Patty Solomon (McMaster University), Kelly O’Brien (University of Toronto), Nancy Salbach (University of Toronto), Sergio Rueda (OHTN and University of Toronto), Brent Oliver (University of Calgary), Lynne Sinclair (Curriculum Consultant, University of Toronto) and Ashley Mollison (Study Coordinator, University of Victoria).
Study funding: Funding for this study was provided by the Canadian Institutes of Health Research (CIHR) through a knowledge synthesis grant and a “Knowledge to Action” grant.
Acknowledgements: We wish to thank our Advisory Committee members for their time and expertise, and thank the participants in the interviews and focus groups for their perspectives on labour force participation for people living with HIV
Module 1
Introduction to Return to Work for People Living with HIV
Welcome to the “Getting to Work” learning modules! The first module has two parts and provides an overview of HIV and labour force participation issues for people living with HIV. It also introduces strategies for supporting clients through these complex issues.
The objectives of this module are to help you:
- To understand some of the unique issues faced by people living with HIV when considering return to work;
- To obtain an overview of important factors that influence labour force participation for people living with HIV;
- To learn an approach to, and strategies for assessment of, labour force participation for people living with HIV.
| General Questions (Please consider these questions on your own in advance of the group discussion) |
|---|
|
Part 1: Understanding the Basics of HIV
Case 1 - Maria
Maria is a 50 year old woman who emigrated from Brazil 10 years ago. She is recently separated from her husband and has 2 children living at home, Alberto, age 20, and Cecilia, age 17. Alberto attends community college and Cecilia is in grade 12. Maria has no post-secondary education but speaks fluent English. She ran her own restaurant when she lived in Brazil. She worked at Miss Chalet restaurant in Canada for several years but quit her job when she was diagnosed with HIV 8 years ago. She has been on provincial disability benefits for 6 years and tells you she wants to return to work as she feels that her health is good and her viral load is “under control”. She comes to see you as she is unsure if she can work. She worries about infecting others and in fact tells you that is why she stopped working after her diagnosis. She also is very concerned about her co-workers discovering her HIV positive status.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
HIV 101
CD4 and Viral Load
- HIV is a disease that attacks the immune system, specifically, the CD4 T-Cells that normally fight infection in the body.
- Two measures of HIV progression are CD4 count and viral load in the blood.
- CD4 count is a measure of immune function – how well the body fights off infections. In a person not living with HIV, CD4 count is normally between 600 to 1200 cells/ mm3 (number of cells per cubic millimetre of blood). In a person who is living with HIV, CD4 counts can drop to below 200 cells/ mm3. CD4 count is also a determining factor in starting antiretroviral treatment, the treatment for HIV/AIDS.
- Viral load is a measure of how much HIV is in one millilitre of blood. Viral load can be used to measure how antiretroviral treatment is working in the body.
- People living with HIV are considered to have an “undetectable” viral load when tests can no longer measure the amount of HIV in the body. This means that HIV is under control in the body. Recent studies suggest that if a person has an undetectable viral load the risk of transmission may be negligible.
- For more information on this topic visit the Canadian AIDS Treatment Information Exchange (CATIE)’s Living with HIV: Starting Points [1]

Antiretroviral Treatment and Adverse Effects
- Antiretroviral treatment, cART (combination antiretroviral therapy) or HAART (highly active antiretroviral therapy) are terms that refer to medications used for the treatment of HIV.
- Antiretroviral treatments prevent HIV from replicating in the body by interrupting HIV infection of the CD4 cells.
- People living with HIV consult with their physicians to determine when to start antiretrovirals, as well as which combination of antiretroviral drugs to take. There are many factors that influence the decision to begin treatment beyond CD4 count and viral load, including the ability to stay on treatment in light of adverse effects (i.e., side effects of medication), pill burden, and personal and socio-economic factors, such as mental health issues or drug use, access to stable housing, and being able to attend physician appointments regularly.
- Adverse Effects associated with medications are a key factor in influencing a person’s ability to stay on treatment. Adverse effects range from minimal to severe. Some of the more common adverse effects can include chronic diarrhea, nausea, weight loss, lipodistrophy (fat redistribution on the face and body), rash and neuropathy (nerve damage).
- Today, for those newly starting treatment for HIV, antiretroviral treatment can be tailored to the individual so that adverse events can be minimized.
- People living with HIV often use other strategies to complement the management of HIV, including good nutrition, exercise, and complementary alternative therapies, such as herbal therapies.
- For more information on this topic visit CATIE’s A Practical Guide to Drug Treatment for People Living with HIV [2]

HIV Transmission and Misconceptions
- Misconceptions about the transmission of HIV, and resulting stigma against people living with HIV, can contribute to a person’s fear of disclosing their HIV status in the workplace.
- HIV can be transmitted through five body fluids: blood, semen (and “pre-cum” fluid), rectal fluid, vaginal fluid and breast milk.
- HIV can be transmitted when one of these fluids with HIV comes into contact with another person’s fluids through activities such as unprotected sex and sharing used needles.
- HIV cannot be transmitted through unbroken skin where these fluids are not present (e.g., shaking hands, toilet seats, kissing, sharing utensils).
- For more information on this topic visit CATIE’s HIV & AIDS: Basic Facts [3]

Working with People living with HIV on Employment Issues
Case 2 - Frank
Frank is a 35 year old gay man who was diagnosed with HIV 12 years ago. He is in a stable relationship with a very supportive partner. Frank worked for a large company in shipping and receiving until a few years ago. He worked shifts, including evenings, and enjoyed the company and his co-workers. He tells you he had a strong work ethic and was proud of his job. He had been able to continue working for many years after being diagnosed with HIV, although in the past 5 years he began having periods of illness and feeling unwell. He tells you that he was often very tired and started to experience tingling and burning in his feet (neuropathy). He went on short term disability benefits about 1 ½ years ago and then on long term disability as he found the pain in his feet was unbearable. He recently changed his HIV medication and the symptoms have subsided somewhat, so he wants to return to work. He tells you he feels isolated and down and says he is “way too young” not to work. He has many worries, however, about returning to work. None of his co-workers know about his HIV status. He fears that he will be forced to disclose his HIV status as he will need to take his medications during the evening shift. He wonders if he can ever return to his previous work due to challenges with his neuropathy and the possibility that it may worsen but worries that he has no other options for a job.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Factors that Influence Labour Force Participation
Six key factors can influence (either facilitate or hinder) labour force participation for people living with HIV.
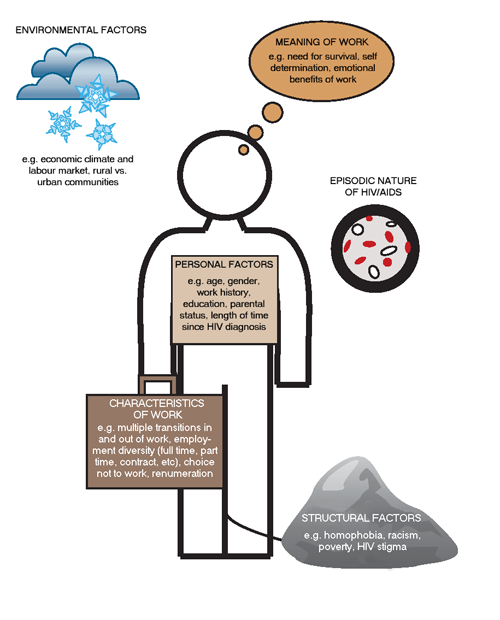
- Environmental factors such as economic climate and location of residence (urban versus rural) can impact the opportunities and the ability for an individual to remain or return to the workforce.
- Structural factors such as stigma and poverty can complicate the ability to participate in the work force.
- The episodic nature of HIV [discussed further in module 3] characterized by sometimes unpredictable periods of wellness and illness can further complicate the ability for someone to remain or return to work.
- Personal factors including age, gender, employment history, and level of education may facilitate or hinder the ability to work.
- Characteristics of work, such as transitioning in and out of the workforce, diversity of employment types (full time, part time, contract work), and remuneration will influence the ability to participate in the workforce.
- Finally, the meaning that individuals place on work, such as the need for survival, self determination, and the emotional benefits tied to work, can also influence the decisions surrounding labour force participation.
Why Does Work Matter?
- Employment is important to help fulfill the basic needs of modern life, including food, shelter, insurance and, possibly, health care benefits.
- For people living with HIV, employment can help lead to increased physical and cognitive stimulation, a reduction in HIV risk behaviours, and possibly even slower disease progression or reduction of HIV symptoms.
- Emotionally, employment can increase self- esteem, increase independence and social connectivity, and provide the opportunity to forge an identity based on one’s career.
- For more information on this topic seeThe HIV and Employment Framework (The Framework) and the Positive Participation Fact Sheet for CBOs/ASOs [4-5]

Barriers to Return to Work
- Income Maintenance: A key barrier for people living with HIV obtaining or returning to work is the potential loss of income, insurance and health benefits associated with leaving income support programs.
- Vocational Factors: Previous unemployment or work interruptions, low levels of job skills, education and training; and poor work/individual matches can be significant barriers to people returning to work, including those living with HIV.
- Health Factors: People living with HIV may experience issues related to medication adherence and complicated scheduling regimes and adverse effects related to their medications (e.g. diarrhea, nausea, rash).
- Mental Health Factors: Emotional and psychological factors, such as depression and neuro-cognitive impairments, which may be cyclical in nature, can act as a barrier for people living with HIV returning to or maintaining employment.
- Social Factors: Social isolation, caregiver responsibilities, stigma and discrimination and a lack of access to social and community benefits play a part in the decision to return to work.
Vocational Rehabilitation 101
Motivation
For those engaged in employment support work, client motivation is a key issue. The motivation to work of people living with HIV is influenced by many personal and structural factors. There are many strategies to address these factors:
- Goal setting is an important element in individual rehabilitation plans. Goals can extend beyond the employment domain (e.g., maintaining supportive personal and family relationships for return to work).
- Strategies to keep clients engaged in employment counselling include offering to schedule appointments close together and to assign homework between appointments.
- An example of a homework assignment – is ask your client to create a mission statement using the following prompts:
- What does an ideal job look like to you?
- What are your values?
- What are your passions?
- Other resources such as the book, “What Colour is Your Parachute” are fun ways for clients to explore their personality types, interests and the way in which they work with others in preparation for return to work or a career change.
For more information on this topic see the resource list at the end of this module [6-9] .
.
Employment Readiness
- You can support your clients to address fears and anxieties related to entering or returning to the work force.
- Fears and anxieties such as those related to being unsuccessful, not being accepted by others and taking on new responsibilities, are common for clients making career changes.
- Additional fears and challenges experienced by people living with HIV, including fears about confidentiality and disclosure of their HIV status, may influence emotional readiness for work.
- For people living with HIV, challenges living with the episodic nature of HIV [discussed further in module 3] including physical and mental health issues, can limit or inhibit employment.
- For more information on this topic see the resource list at the end of this module [5;7]
 .
.
Building Relationships with Employers
- Working with your clients on fears and barriers to work, issues of motivation, employment readiness and retention of employment are one part of the return to work equation. Another aspect is your own practice and ability to build relationships with employers to create opportunities for clients.
- The “open” job market (positions that are listed in public places like newspapers and the internet) account for 20% of the total job market. These jobs are associated with higher competition and can be extremely challenging to obtain for people who have or experience disabilities and who may require workplace accommodations.
- The “hidden” job market accounts for 80% of the total job market. These include “jobs in transition” – people who are retiring, going on maternity leave, etc.
- The hidden job market is accessed through networking, building relationships with employers and becoming a trusted connection for employers. Rather than “uncovering” a job opening, your role can include helping to anticipate a job opening, and if there is a good match between the client and the job posting, introducing the client to the employer.
- For more information on this topic see the resource list at the end of this module [6-9]
 .
.
From the Experts "Things to think about..."
- It is important to understand the barriers that prevent people living with HIV from considering employment. People living with HIV need to be supported to make informed decisions, including the decision not to work. Choice and personal control are key.
- People living with HIV require good job matches that suit their needs and abilities. People living with HIV may require upgrading in the form of job skills, work experience and education.
- Successful return to work and retention of work for people living with HIV can be facilitated by instrumental social supports (peer support and case management); a stable partnership or friend/family support; learning or being supported in self-advocacy skills; and access to community resources (e.g., childcare, transportation, legal support, medical care).
- You can become a connection to employers by understanding the employers’ needs before job openings arise. One idea is to generate a list of employers you would like in your network and set up short meetings with them to get to know their workplace needs. When a job opening arises, you will be in a better position to suggest a client who is a good fit. Another less direct approach is to generate a newsletter highlighting your organization and a few clients that may be of interest to employers.
- Keep in mind the impact that the broader labour market has on your client’s ability to find and maintain employment.
- Organizational culture is important to think about when contemplating employment. People living with HIV or their employment support workers can contact the prospective employer and arrange to have an “information interview” with a human resources professional.

References and Additional Resources
References
- Canadian AIDS Treatment Information Exchange (CATIE). Living with HIV: Starting points. http://www3.catie.ca/eng/LivingWithHIV/startingpoints.shtml
- CATIE. A Practical Guide to HIV Drug Treatment for People Living with HIV. http://www.catie.ca/en/practical-guides/practical-guide-hiv-drug-treatment-people-living-hiv
- CATIE. HIV & AIDS: Basic Facts. http://www.catie.ca/en/practical-guides/hiv-aids-basic-facts
- “Getting to Work” Study. HIV and Employment Framework. http://gettingtowork.hivandrehab.ca/framework.html
- “Getting to Work” Study. Positive Participation Fact Sheet for CBOs/ASOs. http://gettingtowork.hivandrehab.ca/fact_sheets.html
- Bolles, R. N., What colour is your parachute? Ten Speed Press: Berkely, 2012.
- The Hatherleigh Guide to Vocational and Career Counselling. Hatherleigh Press: New York, 1997.
- Dover Training Group & Employment Management Professionals (DGT-EMP). Articles. http://www.dtg-emp.com/articles/list
- Dover Training Group & Employment Management Professionals (DGT-EMP). Motivation. http://www.dtg-emp.com/motivation
Additional Resources
- A resource for people living with disabilities to connect, find and generate answers to employment questions: Episodic Disability Employment Network (EDEN). Persons with Disabilities Online. http://edencanada.ca
- For links to services and information commonly used by people living with disabilities, family members and employers to support people with disabilities in the workplace: Government of Canada. Persons with Disabilities Online. www.pwd-online.gc.ca.
- For information on grants and bursaries for people with disabilities: National Educational Association of Disabled Students http://www.neads.ca/
- A web portal for people living with disabilities, employers or service providers: Workink. http://www.workink.com/
- Employment Action [new site coming in fall 2012]
Module 2
Module 2 - Disclosure & Confidentiality
In the last module, we provided an overview of HIV and introduced the factors that influence labour force participation for people with HIV. This module focuses on the issues of disclosure and confidentiality in the workplace, and provides strategies for talking to employers about these issues.
The objectives of this module are to help you:
- To understand legal and ethical issues related to disclosure of HIV status in the workplace;
- To provide strategies for talking to employers and others about confidentiality and disclosure.
| General Questions (Please consider these questions on your own in advance of the group discussion) |
|---|
|
Case 1 - Damon
Damon is a 29 year old gay male of African descent. He works as a Personal Support Worker in a nursing home in a small rural town. Damon was recently diagnosed with HIV. He has a friend who got fired from his job after he disclosed his HIV status and thus Damon is now fearful of losing his job. Damon trained as a nurse in his home country in Africa; however, he has been unable to find work as a nurse in Canada. He was sponsored by an aunt to come to Canada. He is single and needs a good income to support himself and some family back home. Damon is struggling with long 12 hour shifts and is thinking about asking for shorter work shifts and some work accommodations because of his fatigue.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Stigma and Disclosure
Stigma: Its Layers and Consequences
- In this module, stigma refers to prejudice and discrimination directed at people living with HIV. Stigma can be related to a person’s HIV positive status, gender, sexual orientation, socio-economic status, age or ethnicity.
- Stigma towards people living with HIV is a major factor in decision-making about employment. Disclosure of HIV status can result from a person living with HIV choosing to disclose, or from forced disclosure – where confidentiality is breeched and the person with HIV is “outed” by a supervisor or co-worker, or a person is assumed to be living with HIV by co-workers based on, for example, their appearance or taking sick leave.
- Disclosure can result in the person living with HIV facing stigma and reduced social and professional opportunities.
- People living with HIV may face deeper levels of stigma and discrimination than people living with other health conditions, as the stigma people living with HIV face can be layered with other stigmas, such as stigma related to sexual orientation, mental health issues or poverty. Sub-groups of people with HIV may encounter homophobia and racism that harmfully influence workplace dynamics.
- For more information on this topic see The Positive Participation Fact Sheet for CBOs/ASOs and The Framework [1-2]
 .
.
Disclosure and Support
| Please Note: The legal issues surrounding HIV and employment are complex and vary from jurisdiction to jurisdiction. The following content should not be considered legal advice. For specific legal advice, a professional with an employment law background should be contacted. |
- While forced or inadvertent disclosure occurs in practice, people living with HIV are not required to, and are legally protected from, disclosing their status to employers [3]
 .
. - In the case that a person living with HIV requires workplace accommodations for their needs [discussed further in module 3], the person may need to disclose to the employer the nature of the disability and/or limitations in work abilities. However, people living with HIV are still not required to disclose the specific disability.
- In the case of sick leave, people living with HIV may be required to disclose to their health benefits provider. Benefits providers are required to keep this information confidential.
- If a person living with HIV chooses to disclose to his or her employer, it is important that education for the employer is provided when disclosure occurs. Basic HIV/AIDS resources, such as those listed in Module 1 and other resources for employers at the end of this module can be provided to the employer.
- Due to stigma and discrimination associated with HIV, confidentiality is critical. If a person living with HIV chooses to disclose to an employer, or must disclose to a benefits provider, he or she must be confident that the employer and/or insurance provider keeps this information in strict confidence.
- For more information on this topic see the resource list at the end of this module [4-7](
 .
.
Case 2 - Keith
Keith is a 48 year old male who was diagnosed with HIV 20 years ago. He has been on provincial disability support for most of these 20 years as he thought that an HIV diagnosis meant that he was going to die. Keith had previously worked in retail sales for a small clothing store. He has no education or training beyond high school except for his previous job experience. He is showing signs of muscle wasting and has experienced stigma when out socially due to his physical appearance. Keith is considering return to work, and did apply for one job recently where he was asked if he had HIV. Keith has no pension or savings and is concerned about his future and his financial resources. He has been volunteering at a local ASO. He is currently healthy and has rare periods of episodic illness. Keith wants to keep his diagnosis confidential as he is very concerned about stigma.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Talking with Employers about Stigma
- Those who work with people living with HIV on employment issues may be asked by their clients to intervene with employers and human resources workers regarding stigma.
- If you are communicating to others on behalf of your clients, you need to be clear about your client’s wishes with regard to disclosure to prevent a forced or accidental disclosure.
- If your client does not want you to disclose to the employer, be prepared to tell the employer something like, “We are not at liberty to disclose,” or “That is a personal health issue” should the employer ask about the specific disability.
- Here are a few ideas about how to address stigma in the workplace with employers in a way that is meaningful to them:
- Many employers face significant and sometimes invisible recruitment and retention challenges because of stigma in the workplace. When left unaddressed, stigma against people living with HIV and others can have a negative impact on organizational culture, productivity, competitiveness and reputation.
- Employers may be unaware of these problems within the workplace because HIV-positive employees choose not to disclose their HIV status, fearing a number of negative consequences, including being discriminated against, losing their benefits or even losing their job.
- Basic HIV/AIDS resources such as those listed in Module 1 can dispel myths and misinformation about HIV/AIDS to promote a safer, better-informed, tolerant and respectful workplace.
- For more information on this topic see The Framework and The Positive Participation Fact Sheet for Employers [2;4]
 .
.
Leadership and Peer Support
- If employers are interested in addressing stigma at an organizational level, they can develop HIV/AIDS education and training with the support of their local AIDS service organization [8]
 .
. - Leadership from an organization’s manager or management team and organization-wide human resources support is essential to combat stigma in the workplace [2;4]
 .
. - Basic information about HIV/AIDS can be included in staff orientations and/or diversity training. People living with HIV who have chosen to disclose their status could take a leadership role in developing this training.
- The Opportunities Fund, a government program, provides funding to organizations and businesses for projects that promote labour market participation for people with disabilities [9]
 .
. - At the individual level, people living with HIV would benefit from programs that provide them with the advocacy and leadership skills necessary to contribute to cultural change within their organizations [1,2]
 .
.
From the Experts "Things to think about..."
- For those working on employment issues, the “client” can be the individual living with HIV, the employer and others. There are broader systemic issues that need to be addressed and that will continue to impact labour force participation for people living with HIV, as well as people living with other lifelong, episodic health conditions.
- Those who work with people living with HIV on employment issues play a key role in facilitating a discussion of pros and cons of disclosure in the workplace.
- Making the decision to disclose is often an emotional experience and should be done after thoughtful consideration of personal circumstances and beliefs, as well as consideration of the work environment.
- Providing opportunities for people living with HIV to weigh the options around the decision to disclose (or not to disclose) will help to avoid impromptu status disclosures that can have challenging consequences for a person living with HIV, such as regret and strained working conditions.

References and Resources
- “Getting to Work” Study. Positive Participation Fact Sheet for CBOs/ASOs. http://gettingtowork.hivandrehab.ca/fact_sheets.html
- “Getting to Work” Study. HIV and Employment Framework. http://gettingtowork.hivandrehab.ca/framework.html
- Canadian Human Rights Commission. Policy on HIV/AIDS. http://www.chrc-ccdp.ca/legislation_policies/aids-eng.aspx
- “Getting to Work” Study. Positive Participation Fact Sheet for Employers. http://gettingtowork.hivandrehab.ca/fact_sheets.html
- AIDS Calgary. HIV/AIDS and Employer Rights/Responsibility’s Briefing Document. http://www.aidscalgary.org/files/publications/HIV_EmployersRightsResponsibilities.pdf
- Interagency Coalition on AIDS and Development. HIV/AIDS and the Workplace: Information Sheets for people living with HIV. http://www.icad-cisd.com/pdf/PHA_IS1EN_Employment_info.pdf
- Canadian AIDS Treatment Information Exchange (CATIE). HIV in the Workplace: A Guide for Employers. http://library.catie.ca/PDF/P40/24379e.pdf
- To locate an AIDS Service Organization or other HIV related organization in your area visit ASO 411. http://www.aso411.ca/
- Human Resources and Skills Development Canada. Opportunities Fund for Persons with Disabilities. http://www.servicecanada.gc.ca/eng/of/index.shtml
Module 3-Part 1
Module 3 - Uncertainty
The episodic nature of HIV may result in uncertainty, or worry about the future, for people living with HIV. Individuals may worry about when their next illness might arise, the severity of the illness, and what the outcome might be. In addition, individuals may worry about their income and drug and medical supports.
Uncertainty is a major issue that people living with HIV have to deal with as it may influence a person’s life decisions, such as returning to work, starting a family, starting a new relationship, or moving to a new city. This module is divided into two sections to highlight two key sources of uncertainty for people living with HIV with respect to employment: 1) episodic disability, accommodations and uncertainty, and 2) Income, drug and medical supports, and uncertainty.
The objectives of this module are to help you:
- To gain an understanding of episodic disability and what it means to live with an episodic disability;
- To obtain an overview of issues of accommodation in the workplace;
- To explore income uncertainties for people living with HIV;
- To discuss the impact of episodic illness, and uncertainty associated with income, and drug and medical supports, on return to work and retention of employment.
| General Questions (Please consider these questions on your own in advance of the group discussion) |
|---|
|
Part 1: Episodic Illness, Accommodations and Uncertainty
Case 1 - Becky
Becky is a 58 year old woman who was diagnosed with HIV 15 years ago. She has worked for the past 20 years in a bank in customer service. She has a 30 year old daughter who is very supportive. Becky has had several episodes of acute illness including fatigue and gastrointestinal upset, and needed to take several weeks off work. She has also needed to request increased time off due to frequent medical appointments. Her last episode of illness was longer than previous episodes, and after using up all remaining sick and vacation time, Becky had to go on short-term disability. She wants to maintain her job and her benefits and especially her pension; however, she is concerned about her ability to stand on her feet for long periods of time and her increasing need to take rest breaks. She reports that she is “feeling her age”. Becky has not disclosed her HIV positive status at work. She senses that her work colleagues are upset and frustrated with her about her frequent time off and their need to cover some of her work duties. She is currently feeling good and would like to return to work; however, she is getting pressure now to go on long-term disability or to take early retirement and she is also worried about what would happen with the next episode of illness or need to take time off. Becky is concerned that her younger work colleagues want to take over her job. Her manager has been very supportive in the past, but Becky feels like he is reaching his limit of support for her time off. Becky is wondering if disclosing her status would help him to understand her situation further or if it might risk her losing her job.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Episodic Disability and Employment
- HIV is an episodic disability characterized by unpredictable and fluctuating periods of wellness and illness.
- Other examples of episodic disabilities include multiple sclerosis, arthritis and diabetes.
- The nature of HIV as an episodic disability affects everyone a little differently. Conditions associated with HIV/AIDS, as well as adverse events associated with medications, can result in people living with HIV experiencing “good days” and “bad days”.
- The episodic nature of HIV can be a source of uncertainty for people living with HIV. The episodic nature of HIV can affect the decision-making of people living with HIV around returning to the workforce, as well as some people’s ability to stay in jobs and do their work.
- The availability of workplace accommodations and flexibility can decrease the uncertainty faced by many people living with HIV.
- For more information on this topic see Canadian Working Group on HIV and Rehabilitation (CWGHR)’s Episodic Disabilities web page [1]
 .
.
Talking with Employers about Accommodations
In the previous module, the importance of confidentiality in speaking with employers about stigma was discussed. Confidentiality is also important when speaking to employers about accommodations. The approach that you take with employers will depend on whether or not your client wants to disclose their status.
You may be asked by your client to intervene regarding their episodic disability and need for accommodations with employers and human resource staff. Here are a few suggestions on how to engage in this type of conversation in a way that is meaningful to employers:
- There are difficulties associated with living with an episodic disability including medication scheduling and adverse effects.
- Keeping in mind that the accommodations required by people living with HIV may range from none to significant, Canadian federal Duty to Accommodate legislation requires that employers provide necessary accommodation for people living with episodic disabilities, such as HIV [2]
 .
. - Providing workplace accommodations may increase employee loyalty and reduce employee turnover [3-4]
 .
. - Types of accommodations vary from one person to the next. Workplace accommodations can include time off for doctor’s appointments, flexible schedules, flex time, less physically demanding work, frequent breaks, home-based work or any combination of these [5]
 .
. - For more information to provide to employers see Resources for Employers at the end of this module.
HIV, Employment and Ageing
- With the introduction of antiretroviral medication in 1996, many people living with HIV in North America are living to an older age. Many people with HIV who went through debilitating adverse effects of the early HIV medications did not think they would ever have the opportunity to return to work. Some people living with HIV who exited the labour force because of HIV some time ago, would now be in upper management-type positions had they stayed in the workforce, but are instead starting at the bottom again with outdated skills.
- Ageism can play out in all aspects of the employment process. Employers are less likely to hire older adults, even when they have up-to-date skills and a richer experience. Computer training and skills updating are important for older adults returning to the workforce or changing employment.
- For more information on this topic visit CWGHR’s HIV and Aging resource page [6]
 .
.
From the Experts
From the Experts: "Volunteerism"
- Volunteerism and unpaid placements can help people living with HIV to get a feel for the work they can do and enjoy.
- Volunteerism has great benefits for clients who are contemplating return to work, but are nervous about what they are able to do or taking the risk of leaving public supports. Volunteerism also has benefits for clients who are considering a transition away from the workforce. Some benefits of volunteerism are:
- Providing clients with self-confidence and a sense that they are doing some constructive work
- Providing clients with social contact and reducing social isolation
- Providing the space for clients to assess their capacity for work
- Allowing clients to put something new and current on their resume
- For more information on this topic, related to volunteering within AIDS service organizations see The Living and Serving 3 Study Report [7]
 .
.
From the Experts: Things to think about...
- The episodic nature of HIV can make it difficult for some people with HIV to begin or maintain full time work. Self-assessment is an extremely important component for people living with HIV contemplating, returning to, or finding new employment, or making the decision to stop working.
- If you are assisting a person to find employment, a part of your job may be posing creative solutions to the employer (e.g., assisting the employer to think about carving out a new position that accommodates your client).
- Accommodations are one strategy to assist a person living with HIV to maintain employment. People living with HIV who are already working need to be supported to articulate their needs for workplace accommodation based on their own knowledge of their abilities and limits.
- Functional limitation can be different for everyone. Functional capacity assessments or vocational and neuropsychological assessments are one way to assess functional limitation.
- Your client must also have an understanding of the extent to which the employer is willing to make accommodations (e.g., can the client work part time? Are there lighter duty positions available in the workplace?)
- Fear that another employer will not provide the same accommodations that a person is receiving with their current employer can prevent your client from switching jobs.
- A person’s work experience history, or their current job description, can help inform requests for work accommodations. Professionals who work with people living with HIV can facilitate this conversation.
- In addition to workplace accommodations, there is a need for people living with HIV to have a supportive work environment, to develop fatigue management, energy conservation techniques and pacing strategies [5;9]
 . While these are a few general strategies, effective strategies for maintaining employment need to be client-centred.
. While these are a few general strategies, effective strategies for maintaining employment need to be client-centred.
Module 3-Part 2
Part 2: Income and Uncertainty
Case 2 - Spencer
Spencer is a 25 year old man who was diagnosed with HIV 2 years ago. His CD4 and viral load counts are good and he is feeling physically well; however, he reports good and bad days. He is also showing signs of moderate depression. Spencer is educated as a social worker and graduated from university 2 years ago but has not worked in the field due to his episodic illnesses. He is now fearful of trying to get a job and worried about how he would manage a full work day. Spencer expressed that he is scared about his life expectancy. He does not want to tell his family about his HIV diagnosis, and is most concerned about his new partner and how his diagnosis and uncertain future might impact their relationship. He states that he has little motivation to get a job as he is concerned that he would have to disclose his HIV status. Spencer is on a disability pension now. He worries about whether he will be able to go back on disability if he accepts a full-time job with benefits that he cannot manage. He is often plagued by financial worries. As a social worker, he would need to help support his clients and he is not sure that he has the energy to counsel and work with others at this time.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Income Supports for People Living with HIV
Public Income Supports
People living with HIV may be eligible to receive a variety of income supports, and may be receiving one or a combination of federal or provincial income including:
- Employment Insurance (EI) Sickness Benefit;
- Canada Pension Plan Disability Benefit or Quebec Pension Plan (CPPD/RRQ) Disability Benefit;
- private short or long-term disability insurance;
- and/or provincial and territorial social assistance programs [4;10]
 .
.
See list of income support resources at end of module for more information on each income support.
Private Income Supports
Public Federal Income Supports and Medical Benefits
- Federal income supports include the Employment Insurance (EI) Sickness Benefit and the Canada Pension Plan (CPP) Disability Benefit.
- The Employment Insurance Sickness Benefit provides temporary income, up to a maximum of 15 weeks, to those who are unable to work because of injury or illness. The Canada Pension Plan Disability Benefit is a monthly benefit program for those who are unable to work due to disability.
Public Provincial Income Supports and Medical Benefits
- Provincial income and medical benefits are supports offered through your provincial government. Please see links in the resource section for disability benefits in each province.
- Eligibility and rules surrounding provincial income supports differ from province to province.
Private Income Supports and Medical Benefits
- Private income supports include short-term and long-term disability and are provided by a client’s employer.
- Private income supports vary from workplace to workplace and differ depending on the percentage of an employee’s wage and medical expenses covered.
- Depending on what insurance company the employer uses, there will be different procedures and rules for covering medical expenses.
Income, Drug and Medical Uncertainties
- A major source of uncertainty for people living with HIV is income supports and drug and medical benefits. The strict policies and narrow definitions of benefits programs leave many people living with HIV in a difficult situation. The programs either exclude them from the workforce — even when they are healthy, willing and able enough to be part of it — or give them virtually no choice but to remain in the workforce.
- For people living with HIV who are contemplating employment, the potential loss of public health benefits coupled with the fear of inadequate private health benefits and disability coverage from a new employer, can cause anxiety and act as a disincentive for joining the workforce.
- For people living with HIV with public coverage, returning to work from a leave of absence means running the risk of losing disability benefits and drug coverage that may still be needed. It also raises the possibility that low wages might not provide a level of income comparable to that provided by social benefits.
- For people living with HIV with private coverage, moving from one job to another can be difficult. Having to change insurers, for example, could mean losing extended health benefits coverage — a significant barrier for people living with HIV in terms of career planning and development. For those who are out of the workforce and who rely on long-term disability benefits, there are uncertainties about regaining access to benefits if returning to work is unsuccessful.
- For more information on this topic see The Framework and The Positive Participation Fact Sheet for those Engaged in Policy Work [4;10]
 .
.
Empowering Clients
It is important to work with clients so that they understand and are in control of their employment decisions. Work with your clients to discover their eligibility and rules surrounding the various income and medical supports:
- For those contemplating public benefits, encourage and support your clients to discover the eligibility requirements, such as the minimum EI/CPP contributions needed to have paid, the minimum employment hours needed to have worked (EI), the process for obtaining proof of disability (e.g., physician’s report), and any other criteria to secure these benefits.
- For those on public disability benefits who are considering work, encourage and support your clients to discover rules surrounding these supports such as maximum allowable earnings, the drug coverage of the new workplace (including probationary period), and the process for reinstating public income and benefit supports.
- For those on or contemplating private disability benefits, encourage and support your clients to understand the percentage of their income covered, the need for disclosure of pre-existing medical conditions, percentage of drug costs covered and the procedures for covering medical expenses (e.g., will your client need to pay for their drugs up front?)
Direction for Policy Reform
- Disability policies need to balance potentially conflicting needs in order to provide secure income to those unable to work, and good incentives and supports to those who want and wish to work [9]
 .
. - Increased flexibility of disability income supports would help address challenges related to episodic illnesses such as HIV. The following flexible disability supports are available in some jurisdictions in Canada and are successful at supporting people living with HIV in employment situations:
- Transitional benefits made available to people living with HIV as they manage the process of returning to work helps to minimize the financial risks faced when entering employment or changing jobs.
- The opportunity for automatic reinstatement to income and health benefits in the event of termination of employment provides a safety net for people living with HIV who would otherwise not consider labour force participation.
- Allowable earning amounts are a way for people who are on public disability benefits to remain or return to the workforce. These allowable amounts vary from province to province. See below for a list of provincial disability benefit resources.
- For a more information on this topic and in-depth discussion on directions for policy reform see the resources list at the end of this module [10-12]
 .
.
From the Experts "Things to think about..."
- It is important that people living with HIV are informed about the consequences of leaving current income benefits for return to work due to potential changes to income, insurance and health benefits.
- Knowledge is power. Encourage and support your clients to discover the complex rules surrounding income supports and medical benefits. Individuals will feel more empowered and may feel less uncertain when they are supported to gain their own knowledge about employment in the context of HIV.
- Peer-support is a valuable way for people living with HIV to navigate the system. Connecting and hearing success stories from other people living with HIV who have entered or returned to the workforce after leaving public income and medical benefits is an important way to reduce fears, uncertainties and anxieties about returning to work.

Resources
Income Support Resources
- Federal Employment Insurance Sickness Benefit: http://www.servicecanada.gc.ca/eng/ei/publications/sickness.pdf
- Canada Pension Plan Disability Benefits: http://www.servicecanada.gc.ca/eng/isp/cpp/disaben.shtml
- Quebec Pension Plan Disability Benefits: http://www.rrq.gouv.qc.ca/en/invalidite/Pages/invalidite.aspx
- BC: Information for People with Disabilities http://www.hsd.gov.bc.ca/pwd.htm
- Alberta: Information for Persons with Disabilities http://www.programs.alberta.ca/Living/651.aspx?N=770+175
- Saskatchewan: Office of Disability Issues http://www.socialservices.gov.sk.ca/office-disability
- Manitoba Disabilites Issues Office http://www.gov.mb.ca/dio/
- Ontario Disability Support Program http://www.mcss.gov.on.ca/en/mcss/programs/social/odsp/
- New Brunswick Disability Support Program http://app.infoaa.7700.gnb.ca/gnb/Pub/EServices/ListServiceDetails.asp?ServiceID1=200972&ReportType1=ALL
- Newfoundland and Labrador: Information for Persons with Disabilities. http://www.aes.gov.nl.ca/disabilities/default.html
- Nova Scotia: Services for Persons with Disabilities http://www.gov.ns.ca/coms/disabilities/index.html
- PEI: Supports for People with Disabilities http://www.gov.pe.ca/sss/index.php3?number=1018613
- Yukon: Services for People with Disabilities http://www.hss.gov.yk.ca/disabilites.php
References and Resources
- Canadian Working Group on HIV and Rehabilitation (CWGHR). Episodic Disabilities. http://www.hivandrehab.ca/EN/episodic_disabilities/index.php
- Canadian Human Rights Commission. Resources for Employers including Duty to Accommodate. http://www.chrc-ccdp.ca/portal_portail/employers_information_employeurs-eng.aspx
- “Getting to Work” Study. Positive Participation Fact Sheet for Employers. http://gettingtowork.hivandrehab.ca/fact_sheets.html
- “Getting to Work” Study. HIV and Employment Framework. http://gettingtowork.hivandrehab.ca/framework.html
- CWGHR. Self-Management Fact Sheet on Exercise and HIV. http://www.hivandrehab.ca/EN/resources/documents/Self-managementpamphlet_exercises_June2010_EN.pdf
- CWGHR. Information for Employers: Workplace Accommodation. http://www.hivandrehab.ca/EN/information/employers/workplace_accommodations.php
- Ontario AIDS Network. Living and Serving 3: GIPA engagement guide and framework for Ontario ASOs. http://www.ontarioaidsnetwork.on.ca/upload_image/documents/living_serving_3_oct_2011.pdf
- CWGHR. HIV and Aging. http://www.hivandrehab.ca/EN/agingforum.htm
- CWGHR. Self-Management Fact Sheet on Mental Health and HIV. http://www.hivandrehab.ca/EN/resources/documents/Self-managementpamphlet_MENTALHEALTH_June2010_EN.pdf
- “Getting to Work” Study. Positive Participation Fact Sheet for Those Engaged in Policy Work. http://gettingtowork.hivandrehab.ca/fact_sheets.html
- Canadian HIV/AIDS Legal Network. Support for Survival: Barriers to income security for people living with HIV/AIDS and directions for reform. http://www.aidslaw.ca/publications/interfaces/downloadFile.php?ref=109
- Canadian Working Group on HIV and Rehabilitation. Navigating the Maze: Improving Coordination and Integration of Disability Income and Employment Policies and Programs for People living with HIV/AIDS — A Discussion Paper. http://www.hivandrehab.ca/EN/information/people_HIV/income_security.php
Resources for Employers
- Canadian Human Rights Commission. A guide for employers managing the return to work. http://www.chrc-ccdp.ca/pdf/gmrw_ggrt_en.pdf
- Canadian Counsel on Rehabilitation and Work. http://www.ccrw.org/
- CWGHR. Managing Episodic Disabilities Online: Courses for Human Resources Practitioners. http://www.hivandrehab.ca/EN/information/employers/ManagingEpisodicDisabilitiesOnlineCourse.php
Module 4
Module 4 - Putting it All Together
You have reached the last module in this learning resource. In completing the previous modules, we hope you had the chance to discuss many of the factors involved in working on employment issues with people living with HIV.
This module has a four-part case that deals with one client over a long period of time. We suggest that you discuss each part of the case separately during the session, as each part of the case builds on the previous part. As you work through this final module, please think about the dialogues and information from module 1, module 2 and module 3.
The objectives of this module are to help you:
- To gain an understanding of the process of working with one client over a longer period of time;
- To learn approaches and strategies to working with a complex client with multiple concurrent issues;
- To discuss how to work with potential employers;
- To discuss how to address on the job supports and retention of employment.
| General Questions (Please consider these questions on your own in advance of the group discussion) |
|---|
|
Daniel - Month One
Daniel is a 38 year old man of Aboriginal background who has done some volunteering at the local AIDS service organization. You were asked to speak with him as he expressed some interest, once approached, about the possibility of working. He is friendly, although he appears somewhat reserved and quiet. He was diagnosed as HIV positive 15 years ago. He currently lives in provincial housing and for a time before he moved into his current housing he had lived on the street for several years. He appears to be malnourished and does not look well – with a pale appearance and dark circles under his eyes. He is a heavy smoker and says that he uses drugs occasionally. Daniel is very vague when asked about family support and says that he does not have close friends. He did not finish high school and is receiving provincial disability benefits. When you ask Daniel what skills he has or what work he might want to do, he replies, “I have no skills,” and cannot think of anything that he might be able to do for work. You have a discussion with Daniel about some of the benefits of working. You discuss several ideas and suggestions about what he might do and he seems interested. He says, “Maybe I could work, and that would give me more money that I do need.” He agrees that he will do some preliminary searching and get information and come back to see you in two weeks.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Daniel - Month Six
You have not heard anything from Daniel in the past six months. He did not show-up for your last appointment and did not call to cancel or reschedule. He also stopped going to the local AIDS service organization, but has recently started attending some groups again. The case worker asks you to see Daniel as he mentioned that he wants to talk with you. Daniel does not mention why he did not attend his last appointment but shares that he has had “some personal things going on lately.” He asks you whether there might be some work that he could do soon. He suggests that maybe he could “work under the table” for a few days to bring in some faster income. You decide to give him some specific tasks to do to assess his motivation levels. You ask Daniel to write out a list of the pros and cons of working and going off income support. You also ask him to write a list of potential jobs that he might be able to do. You book an appointment for Daniel to see you next week.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Daniel - Month Seven
Daniel had to cancel his scheduled appointment with you as he was not feeling well. He appears at your office today and asks if he could meet with you. You are able to squeeze in a quick appointment for him. Daniel has brought a list with him that includes the pros and cons of going off income support. He suggests that he could consider some work busing tables at a local restaurant that he frequents. You wonder if it is worthwhile to approach the restaurant owner to consider some part-time work for Daniel.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Daniel - Month Eighteen
You continued to work with Daniel who has now been working full-time busing tables at the restaurant for about six months, with one period where he took a few days sick leave (with notice). You have been in contact with both the employer and Daniel over the integration into the workplace. Daniel is pretty happy, but he worries that he won’t be able to get flex time if needed in the future. Daniel is preparing for a life of unpredictability. You are aware that he will likely need on-going contact and support from you as he navigates future challenges.
| Discussion Questions (Please consider these questions as a group) |
|---|
|
Reflection Points to Consider
This four-part case highlights some of the more complex issues involved in working on employment issues with people living with HIV. While not every case will result in clearly positive outcomes, any work that you do can help to contribute to an individual’s quality of life. How might you define success for Daniel?
In working with people living with HIV, and particularly when working with people with complex issues, it is important to remember that you have community resources to draw upon.
From the Experts "Things to think about..."
- Clients may commonly suggest that they work “under the table.” There are many different perspectives on this and you may have to help the client consider both the short-term and long-term impacts. For clients, “under the table” work may provide needed income and a sense of (re)engagement with the work world. However, if they are on a public or private pension and are caught working without reporting the income, then they could be fined and their benefits may be revoked. If they continue to work and not report, they may not be able to include this work on a resume or list it under job experience on a job application.
- When working with clients, it is important to address issues of job retention early on in the process. Strategically, the earlier your client considers this employment retention piece the better, as it is not something to be addressed only after finding a job. In many cases, this means helping a client with on the job supports, accessing accommodation with employers, replacing a client’s job (e.g., at the end of a contract or where the job is not the right fit) and assisting with career advancement opportunities. Follow-up may involve monthly check-ins with your client for years after the initial meeting.

Conclusion
“Getting to Work” Educational Modules Conclusion
You have reached the end of this learning resource. During the previous four modules, we hope you had the chance to discuss with your colleagues many of the factors involved in working on employment issues with people living with HIV.
- Module One provided you with an introduction to return to work for people living with HIV.
- Module Two discussed disclosure and confidentiality.
- Module Three looked at episodic illness, income, drug and medical uncertainty and the implications for life and work.
- Module Four asked you to put it all together, by considering a more complex case.
Please take a few moments to reflect on what you have learned and how you can apply this to your work environments. This learning resource does not cover all the issues related to employment for those living with HIV, but rather we hope it has focused on several key issues, and provided you with some new knowledge and further resources. You may wish to consider:
- What do you think are the most important things to take away from each module?
- What else do you want/need to learn now?
- Where can you go to help you answer these further questions or ideas?
The fields of health care, HIV, employment issues and education are constantly changing as new knowledge and innovations are developed. We invite you to continue to learn about HIV and employment, from and with your colleagues. Recognizing that resources available vary from jurisdiction to jurisdiction, your work with clients may require collaboration with a variety of organizations and individuals beyond vocational rehabilitation workers and AIDS service organization staff, including income assistance programs, insurance and benefits providers, legal aid, physicians and primary care providers, psychosocial counseling services, addictions/mental health services and human resources personnel.
Collaboration across the many roles and community members who support and help those living with all episodic illnesses will enable a much more comprehensive approach. There are many terrific resources and networks to assist people living with HIV and those who work with them.
Thank you for all your efforts in working on employment issues with people living with HIV. We hope that the content and resources provided here supports your work and your learning.

